Newsroom
Our public affairs team works with news outlets from all over the nation to bring you the latest health care news and information.
For More Information
Director, Media Relations & Communications
303.398.1082 office
303.807.9491 mobile
Email Jessica
Recent Press Releases

National Jewish Health Welcomes Radiologist Brian M. Smiley, MD
New Study Reveals How Burn Pit–Related Particulate Matter Triggers Harmful Lung Inflammation

Dr. Soonho Yoon, International Leader in Thoracic Imaging and Lung Disease Research, Joins National Jewish Health

Study Links Burn Pit Smoke Exposure to Increased Lung Particle Burden in Post-9/11 Veterans

Glen J. Weiss of Vornado Realty Trust Honored at the 57th Annual “A Winter’s Evening Dinner” Dance

Dr. Kristen Steslow Joins National Jewish Health Neurology & Behavioral Health Team

Community Asthma Program on Navajo Nation Increases Care-Seeking for Children with Asthma

Heartburn or Heart Attack: Symptoms Doctors Say You Can’t Ignore

Dr. Sohini Ghosh Joins the National Jewish Health Interventional Pulmonology Team

Rev the Runway Raises More Than $415,000 for National Jewish Health

Dr. Ivana Ilic Joins the National Jewish Health Rheumatology Team

National Jewish Health Expands Lung Cancer Screening Access and Hosts Saturday Screening Event

Dr. Joshua Nardin Joins the National Jewish Health Neurology Team

Study Identifies Viral Combinations That Heighten Risk of Severe Respiratory Illnesses in Infants

National Jewish Health Reaccredited as Pulmonary Hypertension Comprehensive Care Center

National Jewish Health Names Alex Hurst as Executive Director of Health Initiatives
National Jewish Health Earns WASOG Center of Excellence Award for Sarcoidosis

National Jewish Health Receives AHA 100-Year Milestone Award

Study Finds One-Year Change on CT Scans Linked to Future Outcomes in Fibrotic Lung Disease

Dr. Mark Lott Joins the National Jewish Health Behavioral Health Team

Dr. Vivianne Allsop Joins National Jewish Health Rheumatology Team

Dr. Joey Pryor Joins the National Jewish Health Pulmonology Team

Lt. Governor Dianne Primavera and National Jewish Health Host Long COVID Roundtable to Advance Care and Collaboration

Dr. Sarah Rhoads Joins the National Jewish Health Pulmonology Team

Common Cold May Protect Against COVID-19 According to National Jewish Health Researchers
Editorial Urges Deeper Focus on Heart-Lung Interactions in Pulmonary Vascular Disease

National Jewish Health Physicians Recognized as “Top Doctors”

National Jewish Health recognized by U.S. News & World Report as a Top Hospital in Pulmonology

Derek Abbott, MD, PhD, Begins New Role as Chair of Immunology and Genomic Medicine at National Jewish Health

Stay Hydrated: Your Heart Depends On It

Los Angeles Black & White Ball Raises Nearly $500,000 for National Jewish Health

2025 Night & Day Golf Classic Raises Funds for Morgridge Academy at National Jewish Health

Avoiding a Sleepless Summer for Kids Begins in the Morning

New Research Links Skin Barrier Dysfunction to Pediatric Eosinophilic Esophagitis

Legends of Atlanta Gala Raises Nearly $400,000

New Study Identifies Cheek Skin Biomarkers in Infancy That Predict Atopic Dermatitis Before Symptoms Appear

National Jewish Health Researchers Coin New Term ‘Silicosarcoidosis’ to Define Distinct Occupational Lung Disease

Hoops & Hoopla Raises More Than $140,000 for National Jewish Health
National Jewish Health Develops Advanced Molecular Test to Improve Diagnosis of a Genetic Form of COPD

New Research Evaluates the Ability of Patients with Adrenal Crisis to Complete Emergency Cortisol Injections
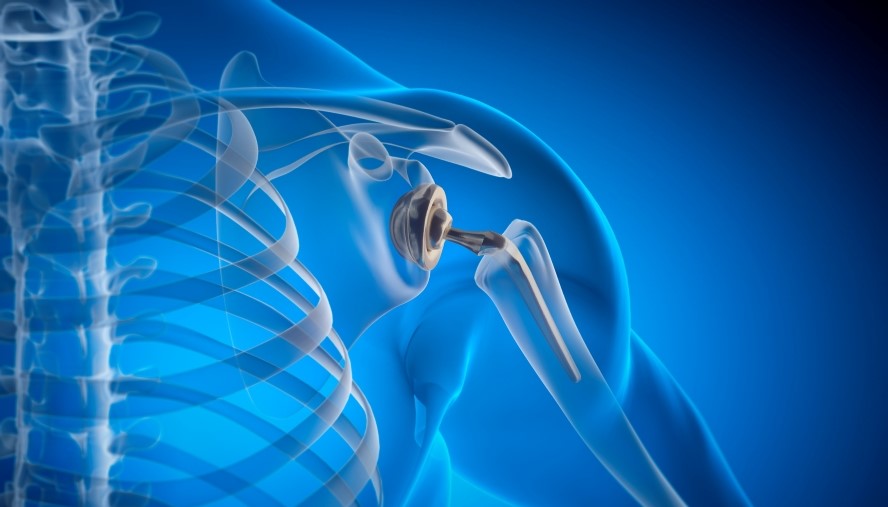
National Jewish Health Led Research Offers Key Insights into Metal Allergies and Impact on Surgical Outcomes for Patients

Lion King-Themed Beaux Arts Ball Raises $2 Million to Benefit National Jewish Health

New Study Identifies Genetic Links between Asthma, Respiratory Inhalers and Air Pollution

National Jewish Health Welcomes Pediatric Pulmonologist Dr. Alicia Della Volpe

Research Shows Positive Impact of CFTR Modulators on Pregnancy Outcomes in People with Cystic Fibrosis

Dr. Daniel Groves Joins National Jewish Health Cardiology Team

New Study Links Dust Storms to Increased Emergency Department Visits in the U.S. Southwest
Browse by year
Multimedia Story Assets
Upcoming Fundraising Events
Upcoming Education Events
March
62nd Annual Denver TB Course (Hybrid Event)
1:30PM
National Jewish Health - Molly Blank Conference Center
1400 Jackson Street, Denver, Colorado 8020662nd Annual Denver TB Course (Hybrid Event)
1:30PM
National Jewish Health - Molly Blank Conference Center
1400 Jackson Street, Denver, Colorado 8020662nd Annual Denver TB Course (Hybrid Event)
1:30PM
National Jewish Health - Molly Blank Conference Center
1400 Jackson Street, Denver, Colorado 80206September
NTM & Bronchiectasis Conference for Healthcare Providers (Hybrid Event)
12:15PM
National Jewish Health - Molly Blank Conference Center
1400 Jackson Street, Denver, Colorado 80206NTM & Bronchiectasis: Patient & Family Conference (Hybrid Event)
9:00AM
National Jewish Health - Molly Blank Conference Center
1400 Jackson Street, Denver, Colorado 80206October
February
49th Annual Pulmonary & Allergy Update
4:00PM
Keystone Conference Center
633 Tennis Club Road, Keystone, Colorado 80435


