Sjögren’s Disease
This information was reviewed and approved by Mehrnaz Maleki Fischbach, MD (3/31/2019).
- Do not delete this
What Is Sjögren’s Disease?
Sjögren's disease (pronounced sho-grins) is a chronic autoimmune disease in which the body's immune system inappropriately attacks one's own tissues, particularly the glands that produce moisture for the eyes, the mouth and elsewhere in the body.
Up to 4 million people in the United States may have Sjögren's disease, making it one of the most prevalent autoimmune diseases. It is unknown exactly what causes the disease, but both genetic and environmental factors are thought to play a role. Sjögren's disease may occur in association with other autoimmune conditions, including systemic lupus erythematosus (also called SLE or just lupus), rheumatoid arthritis or scleroderma (a condition that affects the skin and connective tissue).
Signs and Symptoms
Because Sjögren's disease often targets the tear and salivary glands, the most common symptoms involve the eyes and mouth. Symptoms can appear in a wide array of organs and tissues, though, like in other autoimmune diseases.
Symptoms of Sjögren's disease can include:
- Dryness of the eyes
- Dryness of the mouth
- Difficulty swallowing
- Change in taste
- Frequent cavities in the teeth
- Frequent oral yeast infections
- Swollen salivary glands
- Vaginal dryness
- Heartburn
- Cough
- Shortness of breath
- Arthritis
- Fatigue
Diagnosis
It is often difficult to diagnose Sjögren's disease. In fact, it may take years before a definite diagnosis is made. In order to diagnose the disease, a rheumatologist will use a set of criteria consisting of symptom scores, blood tests, medical history, and other physical criteria and symptoms.
Laboratory Tests
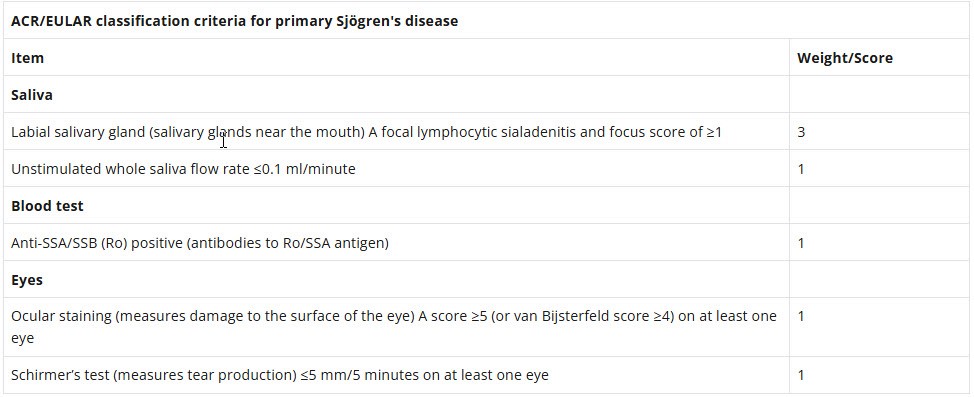
In 2016, the American College of Rheumatology (ACR) and European League Against Rheumatism (EULAR) jointly endorsed a new set of criteria for the classification of Sjögren's disease derived through international consensus. These criteria are based on testing of the saliva, blood and eyes.
The results of these testing will be scored using the following criteria, and evaluated alongside other symptoms and medical history to make a diagnosis. People with a score of 4 or greater and who show symptoms of the disease are generally considered to have Sjögren's.
Treatment
It is important to recognize that there is no cure for Sjögren's disease. In addition, because it is a chronic disease, people often require medical therapy for many years. Goals of therapy will vary for each person, since treatment is guided by the organs that are affected.
Medications
- Artificial tears & eyedrops: Because Sjögren's often targets the eyes, leading to dry eye and other symptoms, treatments can be used to help keep the eyes moist and prevent damage.
- Saliva Stimulants: Saliva stimulants (pilocarpine/Salagen® and cevimeline/Evoxac®) can be used for dryness of the mouth. Artificial saliva tablets may be another option for those with mouth dryness.
- Antirheumatic Medications: Antirheumatic medications are those used for rheumatoid arthritis that help reduce fatigue and joint swelling caused by autoimmune conditions. They may be prescribed by your doctor if you are experiencing joint symptoms or chronic fatigue.
- Immunosuppressants: In severe cases of Sjögren's, where blood vessel damage, nervous system involvement or lung involvement occur, immunosuppressant medications may be needed to control the underlying autoimmune condition and reduce inflammation.
Therapies
Ophthalmologic Procedures: For some people, additional ophthalmologic procedures may be needed to maintain eye moisture if medications are not effective. Regularly discuss any eye symptoms you have with your eye doctor.
Lifestyle Management
A healthy lifestyle is important for everyone, including people with Sjögren's disease. In addition to staying active and eating healthy, it is important to take care of systems commonly targeted by Sjögren's, like the mouth and eyes.
Tooth Care
People with Sjögren's disease are at increased risk for gum disease and infections. See the dentist every 6 months, and follow the steps below to properly care for your teeth and gums:
- Brush your teeth for three minutes at least two times a day. Don’t forget your gums!
- Floss at least once a day. If away from home, use a toothpick to clean between your teeth.
- When you're done brushing and flossing, rinse your mouth with water.
- Replace your toothbrush every three to four months.
Get Checked Regularly
In addition to seeing your regular doctor and rheumatologist, it is recommended to see a dentist every 6 months and an eye doctor every year to help manage mouth and eye symptoms that may occur.
Clinical Trials
Clinical trials help determine new treatment options for diseases and conditions. Patients with Sjögren's disease have access to clinical trials and should speak with their doctor to determine what trials may work best for them.
See a Specialist
If you or a loved one has symptoms of Sjögren's disease, it’s important to be evaluated by a rheumatologist.
At National Jewish Health in Denver, Colorado, we have a dedicated rheumatology program with extensive experience treating Sjögren's disease. Learn more about our program or use the button below to make an appointment.
 Programs and Services
Programs and Services
Thousands of patients come to us from around the world to team with our expert physicians and researchers and seek treatment for respiratory, cardiac, immune and related conditions. Search our treatment programs.
 Clinical Trials
Clinical Trials
For more than 100 years, National Jewish Health has been committed to finding new treatments and cures for diseases. Search our clinical trials.
