FAQs about Metered-Dose Inhalers
This information was reviewed and approved by Ann Mullen, RN, CNS, AE-C, CDE, Deborah A. Fending, RN (1/1/2022).
How do I clean my MDI?
How do I prime my MDI?
How do I use an MDI?
Can I still use a spacer/holding chamber with my MDI MDI?
How can I tell if the MDI is empty?
What You Need to Know About Metered Dose Inhalers
 There are a number of ways to deliver inhaled medication. They include:
There are a number of ways to deliver inhaled medication. They include:
- Metered-dose inhaler (MDI)
- Metered-dose inhaler with spacer/holding chamber
- Dry powder devices
- Soft-mist device
- Nebulizer
This information will focus on the metered-dose inhalers. The table below is a current list of metered-dose inhalers.
How do I clean my MDI?
Cleaning your MDI is important and different depending on the medicine in the MDI. The table below describes how to clean the plastic case for each medicine.
How do I prime my MDI?
Priming is spraying the medicine into the air before you use the MDI. This allows for an accurate dose when you inhale the medicine. MDIs need to be primed before the first dose and when not used for a period of time. Priming your MDI is different depending on the medicine in the MDI. The table below describes how to prime the MDI with each medicine.
Bronchodilator Medicine (short-acting) | ||||
| Medicine Name Atrovent® HFA (ipatropium) | Puffs in canister 200 | Cleaning
| Priming Before first dose: 2 sprays | Other |
| After 3 days of non- use: 2 sprays | ||||
| Medicine Name ProAir HFA (albuterol) | Puffs in canister 200 Dose counter on MDI. | Cleaning
| Priming Before first dose: 3 sprays After 2 weeks of non- use: 3 sprays | Other |
| Medicine Name Proventil® HFA (albuterol) | Puffs in canister 200 | Cleaning
| Priming Before first dose: 4 sprays After 2 weeks of non- use: 4 sprays | Other |
| Medicine Name Ventolin® HFA (albuterol) | Puffs in canister 200 Dose counter on MDI. Replace when counter gets to 000 or 6 months after opening package, whichever comes first | Cleaning
| Priming Before first dose: 4 sprays After 2 weeks of non-use: 4 sprays When dropped: 4 sprays After washing: 1 spray | . Other |
| Medicine Name Xopenex HFA (levalbuterol) | Puffs in canister 200 | Cleaning
| Priming Before first dose: 4 sprays After 3 days of non- use: 4 sprays | Other |
Bronchodilator Medicine (long-acting combination) | ||||
| Medicine Name Bevespi® Aerosphere (formoterol & glycopyrrolate) | Puffs in canister 120 Dose indicator on MDI. Replace when indicator gets to 000 or 6 months after opening package, whichever comes first | Cleaning
| Priming Before first dose: 4 sprays After 7 days of non- use: 2 sprays | Other |
Anti-Inflammatory Medicine | ||||
| Medicine Name Alvesco® (ciclesonide) | Puffs in canister 60 Dose counter on MDI Replace when counter gets to 0. If MDI dropped dose counter may not be accurate.
| Cleaning
| Priming Before first dose: 3 sprays After 10 days of non- use: 3 spray | Other Two doses available (80, 160) Rinse mouth with water, gargle and spit out the water after using the medicine. |
| Medicine Name Asmanex® (mometasone) | Puffs in canister 120 Dose counter on MDI Replace when counter gets to 000. | Cleaning
| Priming Before first dose: 4 sprays After 5 days of non- use: r sprays | Other Two doses available (100, 200) Rinse mouth with water, gargle and spit out the water after using the medicine. |
| Medicine Name Flovent® HFA (fluticasone) | Puffs in canister 120 Dose counter on MDI Replace when counter gets to 000. | Cleaning
| Priming Before first dose: 4 sprays After 1 week of non- use: 1 spray When dropped: 1 spray | Other Three doses available (44, 110, 220) Rinse mouth with water, gargle and spit out the water after using the medicine. Store the MDI with the mouthpiece down. |
Combination Anti-Inflammatory & Bronchodilator Medicine | ||||
| Medicine Name Breztri® Aerosphere (budesonide, formoterol & glycopyrrolate) | Puffs in canister 120 Dose indicator on MDI. Replace when indicator gets to 000 or 6 months after opening package, whichever comes first | Cleaning
| Priming Before first dose: 4 sprays After 7 days of non- use: 2 sprays | Other |
| Medicine Name Symbicort® (budesonide and formoterol) | Puffs in canister 120 Dose counter on MDI Replace when counter gets to 0 (red zone) or 3 months after opening the package whichever comes first. | Cleaning
| Priming Before first dose: 2 sprays After 7 days of non- use: 2 sprays When dropped: 2 sprays | Other Two doses available (80, 160) Rinse mouth with water, gargle and spit out the water after using the medicine. Do not take the unit apart. Store the MDI with the mouthpiece down. |
| Medicine Name Advair® (fluticasone and salmeterol | Puffs in canister 120 Dose counter on MDI Replace when counter gets to 000. | Cleaning
| Priming Before first dose: 4 sprays After 4 weeks of non- use: 2 sprays When dropped: 2 sprays | Other Three doses available (45, 115, 230) Rinse mouth with water, gargle and spit out the water after using the medicine. |
| Medicine Name Dulera® (mometasone and formoterol) | Puffs in canister 120 Dose counter on MDI Replace when counter gets to 000 | Cleaning
| Priming Before first dose: 4 sprays After 5 days of non- use: 4 sprays | Other Two doses available (100, 200) Rinse mouth with water, gargle and spit out the water after using the medicine. |
How do I use an MDI?
Correct technique is important when inhaling your medicine with any device. Take your inhaled medicine with you when you visit the doctor. Your doctor or nurse can watch your technique to make sure you are getting the medicine.
Remember to follow these steps when you use your MDI:
Remove the cap from the inhaler.
Hold the inhaler with the mouthpiece at the bottom.
Shake the inhaler. This mixes the medication properly.
Gently breathe out.
Check which technique your health care provider recommends and follow the step:
Use a spacer/holding chamber – Place the MDI in the spacer holding chamber. Seal your lips around the spacer/holding chamber mouthpiece.
Use open mouth technique - Hold the mouthpiece 1½ - 2 inches (2 - 3 finger widths) in front of your mouth.
Use closed mouth technique – Place the mouthpiece in your mouth with your lips sealed tightly around the mouthpiece.
Tilt your head back slightly and open your mouth wide.
Seal your lips around the mouthpiece (depending on technique you are using listed above).
Press the inhaler and at the same time begin a slow, deep breath.
Continue to breathe in slowly and deeply over 3 - 5 seconds. Breathing slowly delivers the medication deeply into the airways.
Hold your breath for up to ten seconds. This allows the medication time to deposit in the airways.
Resume normal breathing.
Repeat these steps when more than one puff is prescribed.
Can I use a spacer/holding chamber with my MDI?
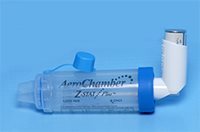 A spacer/holding chamber is a device that is placed between the MDI and your mouth.
A spacer/holding chamber is a device that is placed between the MDI and your mouth.
A spacer/holding chamber can improve your MDI technique. The spacer/holding chamber helps you coordinate the timing of activating the MDI and breathing in. Children and older adults may find it difficult to coordinate the timing and may find a spacer/holding chamber helpful. Anybody may find it difficult to coordinate the timing when having trouble breathing and may find a spacer/holding chamber helpful.
 A spacer/holding chamber can also trap larger particles in the spacer. These particles are more likely to stay in the mouth and cause more side effects.
A spacer/holding chamber can also trap larger particles in the spacer. These particles are more likely to stay in the mouth and cause more side effects.
When using a spacer/holding chamber the spacer/holding chamber should be anti-static. The spacer/holding chamber should also have a one-way valve to help you coordinate the timing of activating the MDI and breathing in. The space in the spacer/holding chamber should be large enough. The AeroChamber® is a common spacer/holding chamber.
How can I tell if the MDI is empty?
The canister of your MDI is marked with the number of puffs (actuations) in the canister. There are more puffs of propellant in the MDI than medicine. The MDI may feel as if there a number of puffs left when you shake the inhaler, but the medicine is gone and only propellant is left. Plan ahead so that you get a new inhaler before the old one is used up.
Many MDIs have a built in counter or indicator to show how long the medicine will last. The numbers count down when a dose is sprayed. When you get to 000 stop using the inhaler and start using a new inhaler. If your inhaler does not have a counter, write the date you start using each inhaler on the inhaler. Place a piece of tape on the plastic case and write the date on the tape. You can calculate when the inhaler will be empty.
Whichever technique you use, remember to figure out how long the medicine will last. Then plan ahead so that you get a new inhaler before the old one is used up.
Whichever device you use, make sure you know:
- How to use the device
- How to tell when the device is empty
- How to clean the device
Also check the package insert that comes with the medicine for more information.
