The human immune response has both a rapid innate component and a slower but more specific adaptive component. The Alper lab is investigating the innate immune response, which involves the action of phagocytic and cytotoxic cells that migrate to the site of infection and that produce antimicrobial compounds. Innate immunity regulates the inflammatory response as well as playing a key role in the activation of adaptive immunity. Thus, a robust innate immune response is critical for fighting infection.
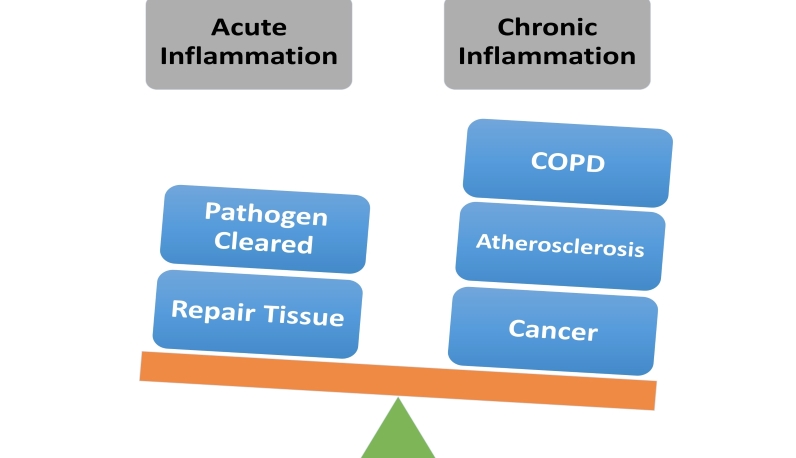
Of course, too much of a good thing is not necessarily good. If the innate immune response becomes activated chronically, then this can contribute to the pathogenesis of many different diseases with an inflammatory component. Thus it is critical not only that innate immunity is activated when needed (upon infection) but that this response is also self-limiting and ultimately inactivated when not needed to prevent disease.
Dr. Alper's laboratory is focused on understanding the regulation of the innate immune response, particularly as it relates to the basis for these inflammatory diseases. The signaling pathways involved in the activation of innate immunity have been studied by numerous labs; in contrast, the pathways that terminate this response are much less understood. The Alper laboratory is investigating two signaling mechanisms that terminate persistent inflammation and therefore prevent chronic inflammatory disease: the regulation of alternative splicing in the Toll-like receptor (TLR) signaling pathway and the subcellular trafficking of TLR signaling pathway components. Understanding how the maintenance of TLR signaling is regulated offers the potential to devise ways to ensure that inflammation is terminated to prevent diseases with an inflammatory component.
We are investigating several inflammatory diseases in this context:
Acute Respiratory Distress Syndrome (ARDS)
Acute Myeloid Leukemia (AML) and the related Myelodysplastic Syndrome (MDS)
While physiologically quite different, these diseases do share the common feature of an over-exuberant inflammatory response.

Scott Alper, PhD
Personnel
Principal Investigator
Faculty Scientist
- Frank Lee, PhD
Postdoctoral Fellow
- Johnathon Schafer, PhD
Laboratory Researchers
- Matthew Lapinig
- Julia Hollaway
Publications
Lee FFY, Harris C, Alper S. RNA Binding Proteins that Mediate LPS-induced Alternative Splicing of the MyD88 Innate Immune Regulator. J Mol Biol. 2024 Feb 17;436(8):168497.
Gurule NJ, Malcolm KC, Harris C, Knapp JR, O'Connor BP, McClendon J, Janssen WJ, Lee FFY, Price C, Osaghae-Nosa J, Wheeler EA, McMahon CM, Pietras EM, Pollyea DA, Alper S. Myelodysplastic neoplasm-associated U2AF1 mutations induce host defense defects by compromising neutrophil chemotaxis. Leukemia. 2023 Oct;37(10):2115-2124.
Lee FFY and Alper S. Alternative pre-mRNA splicing as a mechanism for terminating Toll-like Receptor signaling. Front Immunol. 13:1023567 (2022).
Saleh LS, Amer LD, Thompson B, Danhorn T, Knapp JR, Gibbings SL, Thomas S, Barthel L, O’Connor BP, Janssen W, Alper S, and Bryant ST. Mapping macrophage polarization and origin during the progression of the foreign body response to a poly(ethylene glycol) hydrogel implant. Adv Healthc Mater. 11(9):e2102209 (2022).
Pollyea DA, Kim HM, Stevens BM, Lee FFY, Harris C, Hedin BR, Knapp JR, O’Connor BP, Jordan CT, Pietras EM, Tan AC, and Alper S. MDS-associated SF3B1 mutations enhance proinflammatory gene expression in patient blast cells. J. Leukoc Biol. 110(1):197-205 (2021).
Lee FFY, Davidson K, Harris C, McClendon J, Janssen WJ, and Alper S. NF-kappaB mediates lipopolysaccharide-induced alternative pre-mRNA splicing of MyD88 in mouse macrophages. J. Biol. Chem. 295(18):6236-6248. (2020).
Janssen WJ, Danhorn T, Harris C, Mould KJ, Lee FFY, Hedin BR, D’Alessandro A, Leach SM, and Alper S. Inflammation-induced alternative pre-mRNA splicing in mouse alveolar macrophages. G3. 10(2):555-567.
Lab Activities